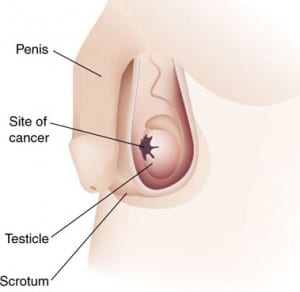
What is testicular cancer?
Majority (more than 95%) of testicular cancers arise from germ cells which are precursors of sperm. They are called as germ cell tumours (GCTs). Germ cells line the tiny tubes (tubules – also called as seminiferous tubules) and undergo a series of proliferation and differentiation to become sperm.
The GCTs are commonly seen in the men aged between 15 to 40 years. They are subdivided into seminomas and nonseminomas (NSGCT) or both based on the appearance under the microscope. They also behave differently in their course. Nonseminomas have different combinations and are as such given the name of the cell subtypes.
Although there is an increase in the incidence of testicular cancer in the western world in the last 50 years it is a rare cancer compared to other cancers in men. The exact causes for this rise are not known. Genetic factors seem to have a role in the development of testicular cancer. The risk for the disease is higher in first-degree relatives of cancer patients than in the general population. There is simultaneous increase in the incidence of all types of germ cell tumours (both seminomas and teratomas).
There is some evidence to suggest that sperm quality has decreased in the same period so there may be sharing of common causative factors for both problems. Apart from undescended testis there is no demonstrable risk factor although testicular cancer in other testis is more common in patients who had previous testicular cancer. Testicular cancer is a disease that predominantly affects young and middle aged men. It is curable even in advanced stages.
The simplest and most effective way to detect any testicular abnormality is to feel the testes systematically (palpation) at regular intervals. Testicular self-examination (TSE) can lead to early diagnosis and treatment of testicular cancer.
What are the manifestations of testicular cancer?
- Heavy feeling in scrotum/testis
- Uneven surface of testis
- Testicular pain
- Testicular swelling: Painless or painful
- Enlargement of breasts (gynaecomastia)
- Shrinkage of testis
Private Treatments For Testicular Cancer London
Our private testicular cancer clinic in London offers various different tests to diagnose your testicular problems – such as blood tests, physical examinations, testicular scans and testicular ultrasounds. Our expert urologists can then offer comprehensive advice and support for the next steps of your treatments for testicular cancer in London. The following information provides insight into the various different services London Urologist offer.
What happens once the testicular cancer is suspected?
If you have seen your general practitioner, they will refer you to a specialist (urologist) or they may arrange an ultrasound (US) scan of the testes when atesticular tumour is suspected. If the US scan proves to be abnormal you will then be referred to the specialist (Urologist). Ultrasound scan is fairly accurate and helpful in diagnosing testicular cancer. Biopsy is not performed because of the fear of spread or seeding of cancer cells.
In the specialist’s clinic you are examined and if testicular tumour is suspected, you will be asked to do some blood tests (tumour markers) and a CT scan. The blood tests include lactate dehydrogenase (LDH), serum tumour markers alpha (α) fetoprotein (AFP), and the beta (β) human chorionic gonadotropin (β-hCG) and routine blood tests such as full blood count and liver function tests.
Serum levels of AFP and/or beta-hCG are elevated in approximately 80% to 85% of patients with NSGCTs, even when the tumour has not spread outside the testis (see below). Patients with pure seminoma may have elevated levels of β-hCG but do not have elevated AFP levels. If AFP is elevated in patients with pure seminoma, then the presence of an NSGCT component is considered.
AFP, β-hCG, and LDH levels are vital in the evaluation and management of patients with testicular cancer. They are used for determining diagnosis, staging, and prognosis and for following response to treatment. Obtaining levels of AFP, beta-HCG, and LDH in patients in whom testicular cancer are suspected is mandatory prior to treatment, as is monitoring of these levels during and after treatment. At this point you have to explore the possibility of preserving your fertility.
Once a diagnosis of cancer is made, the testis is removed along with its attachments. A testicular prosthesis may be requested at the same time.
How do I get to preserve my fertility?
It is important to note that there could be a significant impairment of spermatogenesis (sperm production) existing even before any treatment is started- such patients may not be able to do sperm banking; secondly, combination chemotherapy in testicular cancer has substantial effects on testicular function in particular sperm production, therefore it is likely that almost all patients become azoospermic (absent sperm). It takes about 2-3 years after the treatment for a high degree of recovery of spermatogenesis.
When you decide to freeze your sperm it may be useful to get a quick check of your fertility status by getting some hormone blood tests in addition to semen test. The hormone tests include testosterone (T), follicle stimulating hormone (FSH) and luteinising hormone (LH).
The simplest method is cryopreservation; sperm is collected by masturbation and immediately examined and frozen in a special fluid (preservative) and kept in liquid nitrogen. In the UK, the following blood tests are also required for anyone wishing to store their sperm:
- HIV (Human immunodeficiency virus- that causes AIDS- Acquired Immunodeficiency Syndrome)
- Hepatitis B & C (viral disease affecting the liver)
- Cytomegalo Virus (CMV)
Because of the Human fertilisation and Embryology Authority (HFEA) regulatory requirements special consent forms also have to be completed ahead of the storage. These forms indicate how long you wish to keep the material in storage for, what you wish the frozen material to be used for and what you wish done with the material in the event of your death or if you become incapacitated.
If there are no sperm (azoospermia), there are a number of techniques that could be considered carefully to suit the needs of the patient. In such cases, sometime sperm aspiration with a needle or extracting the sperm directly from the opposite testis can be done. If tumour is present in both testes, healthy testicular tissue could be extracted and preserved after removal of testes.
How is staging of testicular cancer done?
Staging is done with CT scans, tumour markers and on microscopic examination of testis.
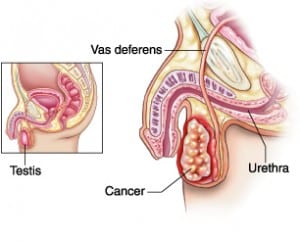
How does testicular cancer spread?
Testicular cancer is spread by three ways in the body:
- Through the surrounding tissue. Cancer invades the tissue surrounding the testis.
- Through the lymphatic system. Cancer cells pass through lymph vessels to other parts of the body. The cells get trapped in the lymph nodes and start growing there. This is the common route.
- Through the blood. Cancer cells escape into the veins and capillaries travelling to other parts of the body.
When cancer cells break away from the original tumour and settle down in other places in the body and start increasing in number rapidly, a second tumours starts (secondary) forming (Metastasis). Different types of tests including CT, MRI and PET-CT scans detect the extent of the spread.
How is testicular cancer treated?
All forms of cancer treatments – radiotherapy, chemotherapy and surgery are used in the treatment of testicular cancer taking into account the type, size, and location of the tumour, metastatic spread and general health. Determining the cell type is important for estimating the risk of metastasis and the response to chemotherapy.
Nonseminoma tumours are more aggressive than seminoma type. When the elements of both seminoma and nonseminoma (mixed) are present the tumour should be treated as a nonseminoma.
Surgical Procedures:
Radical Inguinal Orchidectomy:
The operation involves removal of the affected testis, its cord and dividing the cord at its attachment to the abdominal wall under general anaesthetic. This is the first step in the treatment of all types of testicular cancers. In stage I nonseminoma testicular cancer, blood serum markers should return to normal after this surgery. For very advanced cancer, a radical inguinal orchiectomy may, in rare cases, be delayed until after treatment with chemotherapy has been completed.
The operation is done through a cut in the groin and done as a day care procedure. Removal of the affected testis helps in diagnosing the exact type of the tumour.
It is possible to place a silicone testicular prosthesis in the scrotum. The texture, shape, weight and size of the prosthesis are roughly similar to that of normal testicle. This part of the operation can be done at a later date also after all the treatment is completed. Removing the diseased testis does not affect erection and sexual feelings (libido) if the other testis is normal. Recovery from the operation is swift and only 5-7 days rest is usually required.
Retroperitoneal node dissection (RPLND)
This operation involves removal of the retroperitoneal lymph nodes that lie at the back of the abdomen (retroperitoneum). The lymphatics of each testis travel along the spermatic cord into lymph glands around the large vessels of abdomen (aorta and inferior vena cava). The testicular tumour spreads into the abdomen through lymphatic vessels. There are 2 indications for RPLND.
The first indication is for clinical stage I or IIa nonseminomas and the second being in men with retroperitoneal lymph node masses that remain after completing the course of chemotherapy. In the second, men with nonseminomas who have masses that remain after chemotherapy are surgically removed if the mass is larger than one centimeter and the resection is technically possible (Post-chemotherapy RPLND). In men with pure seminomas and masses that are smaller than 3 centimeters are usually left unoperated but observed for changes with serial CT scans. Traditionally RPLNDs are performed as open procedures using an incision down the middle of the abdomen (midline incision). In selected patients use of laparoscopic RPLND (L-RPLND also called key hole RPLND) is possible mainly performed by experienced surgeons. L-RPLND uses several smaller incisions instead of the one large incision and recovery is much quicker than open procedure.
RPLND for stage I and IIa non-seminomas: Nearly 30% of patients with clinical stage I non-seminoma patients are found to have lymph nodes with cancer which means that they have stage II disease. In the UK chemotherapy is usually preferred to surgery but the patient makes the choice between surgery and chemotherapy when treatment for stage I disease is indicated. The oncologists advise accordingly as to which stage I tumours are at a higher risks of lymph node spread. If the lymph node involvement is present on RPLND, chemotherapy may be necessary to cure the disease. On the other hand if there is no disease is found then an unnecessary chemotherapy can be prevented. However, it is important to remember that the RPLND is a complex operation which requires specialist experience and technical skills in order to remove all of the appropriate lymph nodes and to minimize the side effects of the operation.
Side effects of RPLND:
During the operation there are risks of injury to the intestines, nerves and blood vessels although these are rare. The nerves are known as sympathetic nerves which are responsible for ejaculation of sperm during orgasm. The nerves are specifically looked for and preserved as the injury causes loss of normal ejaculation (retrograde ejaculation). The surgeon discusses in detail about this complication prior to the operation. During recovery bowel movement can become sluggish (ileus). Important complications to look for are deep vein thrombosis and pulmonary embolism.
RPLND to remove residual tumours after chemotherapy. RPLND performed after chemotherapy is a more difficult operation and is more likely to result in retrograde ejaculation. But it is a properly planned procedure and completed in a systematic fashion. Nearly 40-50% of the masses contain dead tumours. In rest of the patients there may be teratoma or one of subtypes of germ cell tumours. In such cases, further chemotherapy may be required. The side effects and complications are already described. In addition there may be complications associated with lungs and deep vein thrombosis. Sometimes lymph may collect in the abdomen (2-3%).
Other types of operations required to remove tumours remaining after chemotherapy: Lung and liver operations may be required by experienced surgeons.
Active Surveillance:
In low-risk clinical stage 1 seminomas and non-seminomas active surveillance is an option after radical orchidectomy. This avoids chemotherapy, radiotherapy or further surgery and their side effects or complications. Serum markers should be normal before the operation or return to normal after radical orchidectomy to consider active surveillance. After orchidectomy a referral is made to the oncologist who would discuss or recommend this approach if they felt that this management is possible. In active surveillance, the patient is monitored by blood tests and scans and the treatment begins only if there is a recurrence of cancer.
This option involves regular doctor appointments for CT scans, chest x-rays, and physical examinations, and blood tests for tumour markers at definite intervals. Both oncologist and patient need to work together in planning the surveillance.
Chemotherapy:
In this method drugs that are designed to kill cancer cells are used. The drug reaches all the cancer cells in the body through the bloodstream. The drugs are used in combination and at different times so that the cancer cells are attacked in different ways. There are definite ways of giving these drugs in cycles. The combination is known as BEP consisting of drugs bleomycin, etoposide and cisplatinum. The side effects of chemotherapy are usually limited to the period chemotherapy is received but some side effects could last for a long time. The effects depend on the individual patient and the dosage used.
Side effects of Chemotherapy:
| Nausea and vomiting | Common side effect; Medications are given to prevent this side effect |
|---|---|
| Fatigue & tiredness | This occurs because of the effects of drugs on normal cells also |
| Hair loss | Usually seen 3-4 weeks after chemotherapy but grow back few months after stopping chemotherapy |
| Anaemia | Drugs could affects cells that produce red cells, white cells and platelets Platelets are necessary for blood clotting so this may be impaired White cells fight against infections so reduction in their number may make the person prone for infections |
| Hearing loss | This is usually a permanent side effect; there may be tinnitus (ringing in the ears) |
| ‘pins and needles’ or numbness | Because of the nerve damage- likely to recover partially or totally but can be permanent |
| Kidney damage | Chemotherapy can affect kidney function but usually reversible |
Radiation Therapy
This involves using high energy radiation to kill cancer cells by damaging their DNA. Radiotherapy is given in patients with early stages of seminomatous tumours (Stage I and IIa and limited stage IIb). Seminomas are sensitive to radiation. Side effects are rare due to lower dosage of radiation but nausea and vomiting are not uncommon. Diarrhoea may also occur.
Recurrence /Relapse
There is 70-80% response to first line chemotherapy and surgery (RPLND or other procedures). Remaining 20-30% of patients will have a disease that does not respond or partly responds to chemotherapy. The oncologist will advise about the treatment and any drug trials that are available. Surgery may be required to complete the treatment.
Life after testicular cancer treatment
Patients with testicular cancer are young and have a high cure rate which means late toxicities are a major concern. The long term side effects include fertility problems, nerve damage, kidney damage and lung problems.
Useful links: www.macmillan.org.uk
This information is not a substitute for clinical assessment and treatment. This is an educational material and advice from your general practitioner or specialist is extremely important!
Treatments For Testicular Cancer London
If you are facing testicular cancer related problems – contact London Urologist today to see how we can help and support you.

Mr Vinod Nargund is a Consultant Urological Surgeon specialising in Urological cancer, male sexual and fertility problems. He was trained in Urology at the City Hospital Belfast, the Royal Infirmary Bradford and the Churchill and John Radcliffe Hospitals in Oxford. You can view all of his qualifications on his biography page.